Amelogenesis Imperfecta
This is an ectodermal disorder and therefore affects the enamel only. The incidence ranges from .01% to .14% depending on the population At least 18 subtypes (Witkop, CJ, 1988) have been identified based on clinical features, light microscopic appearance and the inheritance pattern. This defect affects both the primary and secondary dentitions. Multiple modes of inheritance including autosomal dominant and autosomal recessive are possible.
Features of amelogenesis imperfecta include openbite due to attrition, eruption may be normal or late and the dentinoenamel junction is scalloped. Affected teeth are discoloured (exogenous pigment) and may be pitted, rough or smooth enamel. Enamel is thin or mottled radiographically. Problems include aesthetics, abrasion, sensitivity and caries susceptibility. Pathogenesis is a progressive, functional defect of ameloblasts. Management may include crowns (full coverage) and possibly full mouth osteoplasty (recontouring of bone) to increase the length of the clinical crowns for retention of full veneer crowns.

Pitted form of amelogenesis imperfecta
(courtesy of Drs. Steve Ahing and John Perry, University of Manitoba).
|
|

Snow-capped form of amelogenesis imperfecta (courtesy of Drs. Steve Ahing and John Perry, University of Manitoba).
|
|
A case study of a Type IE X-linked (dominant) smooth hypoplastic amelogenesis imperfecta (Witkop's classification) is presented to illustrate the inheritance pattern of one type of amelogenesis imperfecta. This subtype of AI (amelogenesis imperfecta) was diagnosed through the use of a pedigree and examination of all the members of the M family. The father Chris M had severe, generalized hypoplastic defects of the enamel. A pedigree illustrated that this defect was only transferred to the female children (Katrina M and Maria M). Son Marcus M had a normal dentition. The defects in the teeth of the female children were somewhat less severe than in the father but resulted in vertical banding of the enamel. A diagnosis of Type IE X-linked (dominant) smooth hypoplastic amelogenesis imperfecta was made based on a pedigree and clinical examination of all family members. The pattern of enamel defects in the family are illustrated below.
|
|
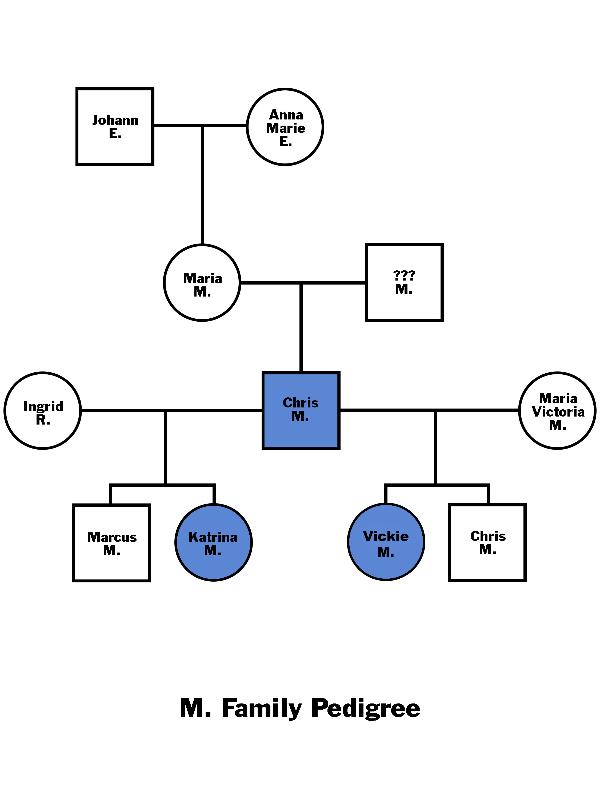
|
Chris M

Amelogenesis Imperfecta
Father Chris M as he initially presented. Maxillary teeth had been treated with metal ceramic crowns. Mandibular teeth are virtually devoid of enamel (courtesy of Dr. BM Cleghorn, Dalhousie University).
|
|
 Occlusal view of Chris M illustrating normal tooth morphology and hypoplastic enamel Occlusal view of Chris M illustrating normal tooth morphology and hypoplastic enamel
(courtesy of Dr. BM Cleghorn, Dalhousie University).
|
|
Right BW radiograph
Chris M
(courtesy of Dr. BM Cleghorn, Dalhousie University).
|
|

Left BW radiograph
Chris M
(courtesy of Dr. BM Cleghorn, Dalhousie University).
|
|

Right PA radiograph
Chris M
(courtesy of Dr. BM Cleghorn, Dalhousie University).
|
|

Left PA radiograph
Chris M
(courtesy of Dr. BM Cleghorn, Dalhousie University).
|
Katrina M
|
|
 Pre-treatment frontal view of daughter Katrina M aged 12 years 9 months Pre-treatment frontal view of daughter Katrina M aged 12 years 9 months
(courtesy of Dr. BM Cleghorn, Dalhousie University).
|
 Maxillary left quadrant close-up of vertical banding of enamel in patient Katrina M illustrating severely hypoplastic enamel Maxillary left quadrant close-up of vertical banding of enamel in patient Katrina M illustrating severely hypoplastic enamel
|
|
|
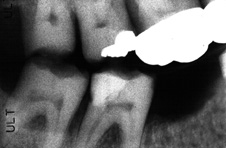
Right BW radiograph
Katrina M
(courtesy of Dr. BM Cleghorn, Dalhousie University).
|
|
|
|
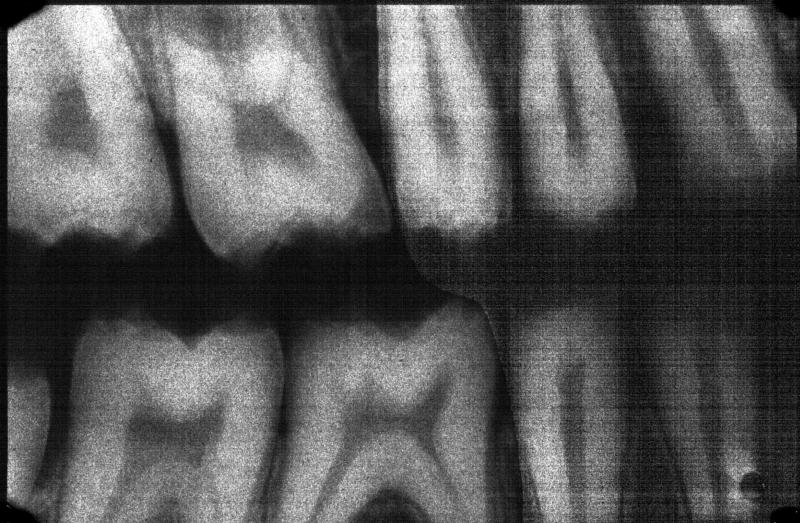
 Left BW radiograph Left BW radiograph
Katrina M
(courtesy of Dr. BM Cleghorn, Dalhousie University).
|
|
|
|
 Post-treatment frontal view of Katrina M Post-treatment frontal view of Katrina M
(courtesy of Dr. BM Cleghorn, Dalhousie University).
|
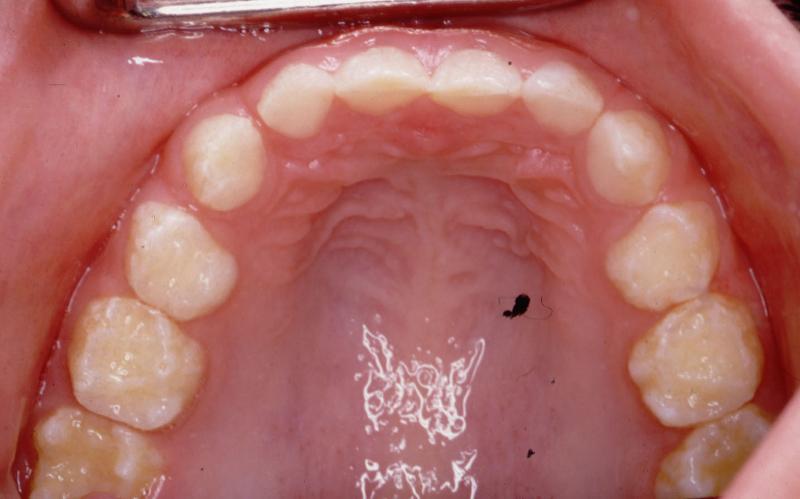
 Post-treatment view of maxillary arch of Katrina M with full coverage of all teeth Post-treatment view of maxillary arch of Katrina M with full coverage of all teeth
|
|
Vickie M
|
|
|
|
 Pre-treatment frontal view of Vickie M aged 5 years 4 months Pre-treatment frontal view of Vickie M aged 5 years 4 months
(courtesy of Dr. BM Cleghorn, Dalhousie University).
|
 Pre-treatment view of maxillary left quadrant of patient Vickie M Pre-treatment view of maxillary left quadrant of patient Vickie M
|
|
|
 Pre-treatment occlusal view of maxillary arch of Vickie M Pre-treatment occlusal view of maxillary arch of Vickie M
(courtesy of Dr. BM Cleghorn, Dalhousie University).
|
 Pre-treatment occlusal view of mandibular arch of Vickie M Pre-treatment occlusal view of mandibular arch of Vickie M
|
|
Marcus M
Marcus and brother Chris Jr. were unaffected by this sex-linked Type IE X-linked (dominant) smooth hypoplastic amelogenesis imperfecta.
|
|
|
|
 Frontal view of Marcus M Frontal view of Marcus M
(courtesy of Dr. BM Cleghorn, Dalhousie University).
|
|
|
|
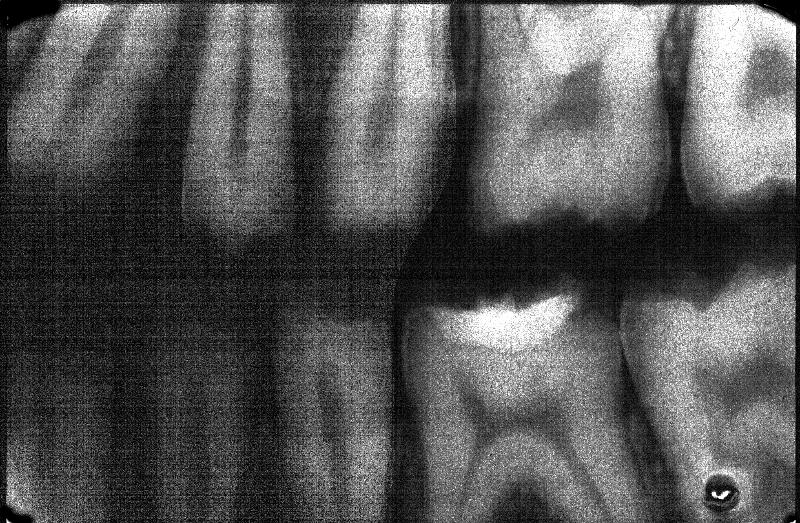
 Right BW Right BW
Marcus M
(courtesy of Dr. BM Cleghorn, Dalhousie University).
|
|
|
|
 Left BW Left BW
Marcus M
(courtesy of Dr. BM Cleghorn, Dalhousie University).
|
|
|
Chris Jr.
|
|
|
|
 Frontal view of Chris Jr. aged 3 years 5 months Frontal view of Chris Jr. aged 3 years 5 months
(courtesy of Dr. BM Cleghorn, Dalhousie University).
|
|
|
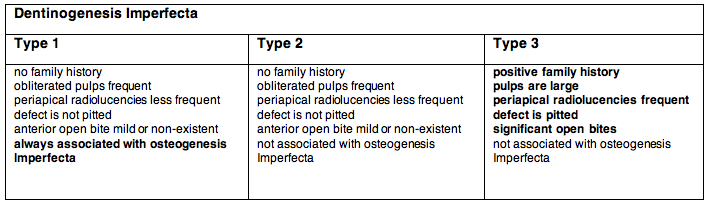
Dentinogenesis imperfecta
This is a mesodermal defect that affects the dentin. The condition is also called hereditary opalescent dentin and can be seen in isolation or associated with a systemic defect (osteogenesis imperfecta). Both the primary and secondary dentitions are affected. Dentinogenesis Imperfecta (DI) is a genetic disorder with an autosomal dominant mode of inheritance. The teeth are blue or brown and translucent. The incidence is approximately 1 in 8,000 in the USA. The classification system for this entity is less than perfect.
Common Features of Dentinogenesis Imperfecta
all teeth are discoloured (types 2 and 3 more prominent)
bell-shaped crowns
attrition
obliteration of root canals in Type 1 and 2 (more marked in the permanent dentition)
enamel is lost early in Types 1 & 2 due to a defect in the DEJ (no scalloping of the DEJ)
difficult to differentiate Types 1 and 2 clinically and radiographically
Type 1 is always associated with osteogenesis imperfecta while Type 2 is never associated unless by chance
 Frontal view of dentinogenesis imperfecta (courtesy of Drs. Steve Ahing and John Perry, University of Manitoba). Frontal view of dentinogenesis imperfecta (courtesy of Drs. Steve Ahing and John Perry, University of Manitoba).
|
|
|
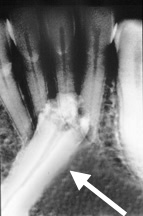
 PA radiograph of dentinogenesis imperfecta illustrating bell-shaped crown on mandibular first molar (courtesy of Drs. Steve Ahing and John Perry, University of Manitoba). PA radiograph of dentinogenesis imperfecta illustrating bell-shaped crown on mandibular first molar (courtesy of Drs. Steve Ahing and John Perry, University of Manitoba).
|
|
|
Occlusal view of a patient with dentinogenesis imperfecta illustrating the severe attrition of all of the maxillary teeth (courtesy of Drs. Steve Ahing and John Perry, University of Manitoba).
|
|
|
 BW radiograph of dentinogenesis imperfecta illustrating obliterated pulps (courtesy of Drs. Steve Ahing and John Perry, University of Manitoba). BW radiograph of dentinogenesis imperfecta illustrating obliterated pulps (courtesy of Drs. Steve Ahing and John Perry, University of Manitoba).
|
|
|
 PA radiograph of dentinogenesis imperfecta illustrating shell teeth (courtesy of Drs. Steve Ahing and John Perry, University of Manitoba). PA radiograph of dentinogenesis imperfecta illustrating shell teeth (courtesy of Drs. Steve Ahing and John Perry, University of Manitoba).
|
|
Impacted Teeth
These are teeth that are prevented from erupting by some physical barrier. The aetiology can be due to a lack of space (crowding) or a rotated tooth germ (so that the tooth is 'aimed' in the wrong direction).
Most Common Impacted Teeth
third molars
maxillary canines
premolars
supernumerary teeth
|
|
|
 PA of impacted permanent mandibular right third molar (courtesy of Drs. Steve Ahing and John Perry, University of Manitoba). PA of impacted permanent mandibular right third molar (courtesy of Drs. Steve Ahing and John Perry, University of Manitoba).
|
|
|
 PA of impacted permanent mandibular right canine; the crown is undergoing resorption (courtesy of Drs. Steve Ahing and John Perry, University of Manitoba). PA of impacted permanent mandibular right canine; the crown is undergoing resorption (courtesy of Drs. Steve Ahing and John Perry, University of Manitoba).
|
|
|

Panoramic radiograph of impacted third molars; the maxillary right third molar is both impacted and inverted; both of the mandibular third molars exhibit a 90 degree horizontal rotation (courtesy of Dr. BM Cleghorn, Dalhousie University).
|
|
|

Panoramic radiograph of a patient with multiple impacted and supernumerary teeth (courtesy of Dr. BM Cleghorn, Dalhousie University).
|
|